Enhancing Patient Care with the My Irrigation Booklet (MIB): A Resource for Patients, Peace of Mind for Healthcare Providers
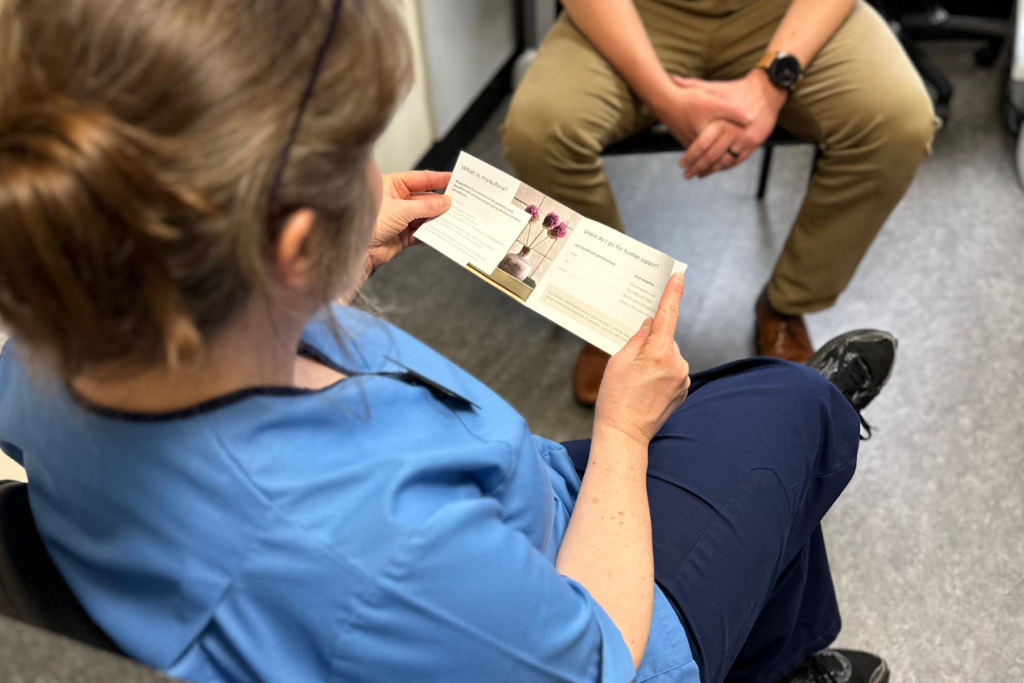
In the ever-evolving landscape of healthcare, effective communication and patient education are integral to ensuring optimal outcomes. The new My Irrigation Booklet (MIB) is compact yet powerful tool designed to assist patients in retaining vital information related to beginning rectal irrigation. Understanding the Link between Memory and Adherence: Leys et al. (1995) highlighted that understanding […]
Kim and Steve’s resilience through change

https://youtu.be/dRe_VP0hZjE The beginning of their journey Nineteen years ago, Kim’s life took an unexpected turn when a spinal cord injury left her reliant on a wheelchair and facing the challenges of double incontinence. This marked the beginning of a journey filled with adaptation and resilience. Fourteen years later, Kim received another life-altering diagnosis: early-onset Alzheimer’s. […]
Finding what works for you?

By Andy Hamilton, Head of Marketing at Qufora Ltd An electric car, treatment pathways and a couple’s devotion to each other. Shooting one of our personal stories is important to us as we know the difference they can make to people managing their own bowels and situations. It can be the catalyst for them to […]
Bladder & Bowel UK Professional Symposium – North West 2024 Round Up

By Michelle Henderson, Clinical Education Manager It was a pleasure to attend the BBUK symposium in Bolton this month. The venue was packed and, as always, BBUK had come up trumps with an excellent agenda for both adult and paediatric bladder and bowel specialists. To ensure you don’t miss out on the latest updates […]
Association for Continence Advice (ACA) Annual Conference and Exhibition 2023 Round Up

By Brigitte Collins, Global Clinical Education Manager The team at MacGregor Healthcare had the pleasure of attending the Association for Continence Advice (ACA) conference on 15/16th May at the National Conference Centre, Birmingham. Once again ACA have triumphed in what was a very well organised conference. The programme was packed full of presentations that slotted […]
Low Anterior Resection Syndrome (LARS) Masterclass 2023 Round Up
By Brigitte Collins, Global Clinical Education Manager As always, the St Mark’s Academic Institue, Low Anterior Resection Syndrome (LARS) Virtual Masterclass held on the 18th May was well organised with up-to-date material that can be adopted in clinical practice. The annual masterclass aims to equip healthcare professionals with a comprehensive understanding of LARS, including its […]
MS Trust Annual Conference 2023 Round Up
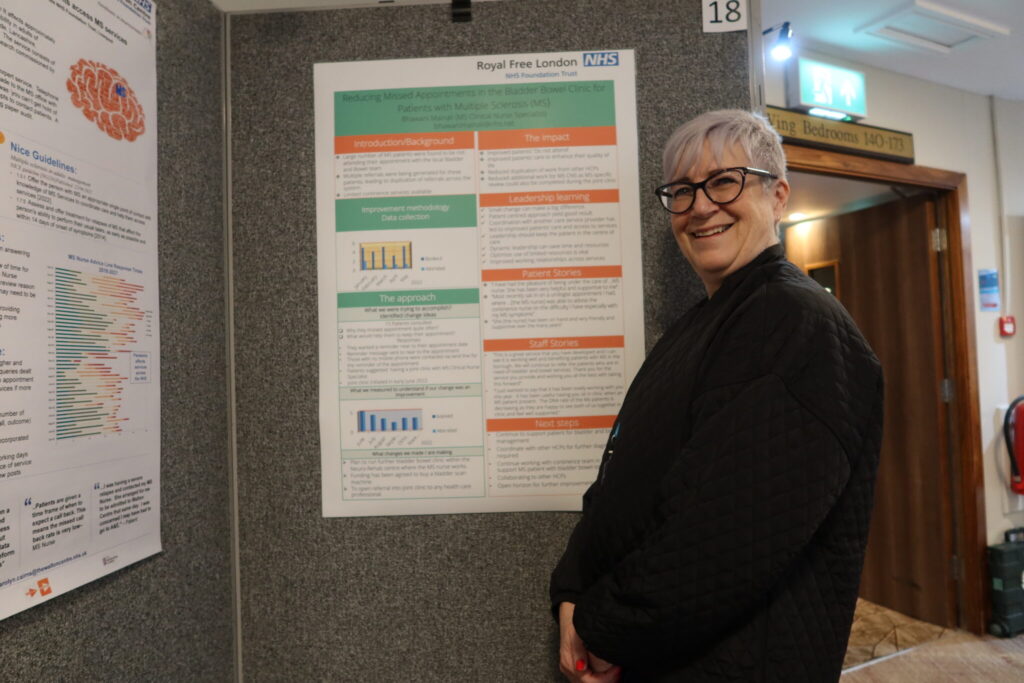
By Brigitte Collins, Global Clinical Education Manager The MS Trust conference gave us the opportunity to share our expertise and knowledge around the Qufora IrriSedo range, discuss case studies and talk with healthcare professionals to understand bowel treatment pathways for multiple sclerosis (MS) as well as ways of improving care. Attending the ‘Developing a consensus […]
Building a support system: The myqufora Support Team’s personalised approach to patient care

By Michelle Henderson
‘Using transanal irrigation for functional bowel disorders: an observational study’ – part 2

Michelle Henderson How do the key findings impact on clinical practice? The PERSPECTIVE* study used an online questionnaire to explore how people with different functional bowel disorders use transanal irrigation. Yan Yiannakou and Michelle Henderson led the study whilst working together in Durham. *PERSPECTIVE: Patient pERSPective of functional bowel disorders: Effects on lifestyle, experienCe of […]
A step-by-step Decision Guide for rectal irrigation
Since the first randomised controlled trial in 2006 of ‘Transanal Irrigation (TAI) in Neurogenic patients’ (Christensen et al, 2006), TAI has become a well-established therapy for patients with refractory faecal incontinence and constipation. A greater range of products have now evolved and choosing the right product for the patient can feel overwhelming and sometimes challenging. […]
myqufora team training

By Michelle Henderson The myqufora team support patients with their rectal irrigation system, wherever they are on their irrigation journey, from the start or over a matter of months. They can help supplement patients initial teaching as the team are able to deal with specific questions often related to the patients individual circumstances. This helps […]
‘Using transanal irrigation for functional bowel disorders: an observational study’

Summary by Michelle Henderson INTRODUCTION: The PERSPECTIVE* study has examined the burden of a wide range of functional bowel disorders (FBDs) on lifestyle including quality of life, work productivity and healthcare utilisation. FBDs include all types of irritable bowel syndrome (IBS), functional constipation and functional diarrhoea alongside evacuatory dysfunction and faecal incontinence. In clinical practice, […]

